Abstract
Introduction:
Myeloid sarcoma (MS) is the involvement of acute myeloid leukemia (AML) cells in extramedullary tissues, whose mechanism remains to be further elucidated. How MS affects AML prognosis at a molecular level is also an open question. This unexplained tropism of leukemic blasts to extramedullary tissues is likely caused by the combination of genetic and epigenetic aberrations. Our study investigated the paired samples of myeloid sarcoma tissue and bone marrow (BM) at diagnosis in perspective of elucidating specific genetic abnormalities that underpin the ectopic homing of MS cells.
Methods:
A 62-patient cohort of pathologically-proven MS diagnosed between 2005-2018 was systemically reviewed. Histomorphology and immunophenotypes of all cases were reviewed by the hematopathologist. Cytogenetic karyotyping in BM cells was carried out with conventional G-banding method. Twenty-five cases of extramedullary presentation at initial diagnosis were further interrogated with next generation sequencing. DNA was extracted from formalin-fix-paraffin-embedded (FFPE) tissue using an error-avoiding reagent against formaldehyde-caused artificial single nucleotide changes (QIAGEN GeneRead). Mutations in 54 genes associated with myeloid disorders were analyzed in Illumina MiSeq sequencer along with the TruSight Myeloid Sequencing Panel. FLT3-ITD in bone marrow was detected by Sanger sequencing. Of these, 16 patients' paired samples (16 FFPE tissue and 16 BM tissue) were analyzed in comparison.
Results:
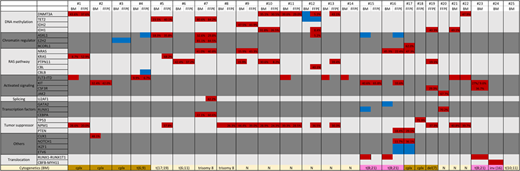
MS occurred concomitantly with leukemic marrow in 21 patients, without bone marrow disease in 2 patients, and resulted from transformation of MPN or MDS/MPN in 2 patients. The median age of diagnosis is 45 years (range 17-72 years), and the male to female ratio is 1.28. Twenty patients received standard treatment with systemic chemotherapy, and nine patients underwent subsequent allogeneic transplantation. The median overall survival was 31.6months ± 20.83 months with a median follow up of 28 months. Cytogenetic patterns included 9 patients with normal karyotypes, 5 with complex changes and 4 with a core-binding factor aberration. The median of mutation numbers in MS was three (range 0- 5) per case. In agreement with prior reports, the most common molecular abnormality in MS was NPM1 (11/25, 44%), followed by FLT3-ITD (7/25, 28%) and DNMT3A (6/25, 24%). The coexisting genetic alterations in the BM from patients without evident AML in morphology or immunophenotypic analyses, suggesting a role for clonal hematopoiesis in the BM. All of the cases with RUNX1-RUNX1T1 translocation harbored KIT mutation. Nineteen out of 25 cases (76%) had a mutation in the genes of receptor tyrosine kinase (RTK)- RAS pathway. In MS-BM paired samples, additional driver mutations in the MS samples included DNMT3A, IDH1, ASXL1, KRAS, CBL, NPM1, KIT and U2AF1. Conversely, one patient's BM PTPN11 mutation was lost in his MS lesion. For more details, the cytogenetic changes, mutational profile and the variant allele frequency were summarized in Figure 1.
Conclusion:
Interestingly, additional driver mutations were identified in the MS samples compared to the BM counterparts, suggesting that a comprehensive characterization of AML heterogeneity might need the mutational profiling of the coexisting MS. AML patients with MS infers a negative prognosis and were treated with frontline allogeneic stem cell transplantation whenever possible in this study. Consistent with prior report, this study showed a higher incidence of genetic alteration of NPM1, FLT3-ITD and DNMT3A in MS along with an enrichment of RTK-RAS signaling pathway mutations. Functional study is needed to delineate the biology underlying the ectopic homing of these commonly mutated genes in AML.
(Figure legend)
Molecular signature of 25 patients with myeloid sarcoma. Highlight in red represents pathologic mutation, highlight in blue represents mutation of unknown significance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal